OVERVIEW OF BONE FRACTURES: CLASSIFICATION, CAUSES, AND TREATMENT METHODS
I. Overview of Bone Fractures
A fracture is a condition characterized by a disruption in the anatomical continuity of a bone, which may be partial or complete, caused either by mechanical forces exceeding the bone’s strength or by pathological processes that weaken its structure.
II. Classification of Bone Fractures
Bone fractures can be classified in various ways:
2.1 By the Nature of the Fracture
- Incomplete fracture: The bone is partially damaged but its continuity is not completely lost.
- Complete fracture: The bone is completely broken or shattered into two or more pieces, resulting in a total loss of continuity.
2.2 By the Condition of Surrounding Soft Tissue
- Closed fracture: A fracture that does not create an open wound connecting the fracture site to the external environment.
- Open fracture: Occurs when the broken bone pierces through the skin, creating an open wound and exposing the bone and surrounding tissues.
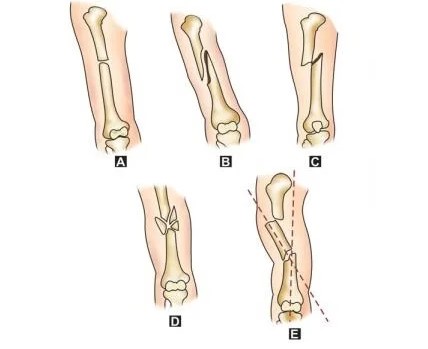
2.3 By the Fracture Line Pattern
- Transverse fracture: The fracture line runs horizontally at a 90° angle to the bone shaft. This type often results from a direct external force or pathological bone weakening.
- Spiral fracture: The fracture line spirals around the bone, usually caused by a twisting force. The bone ends are often sharp and elongated, making alignment and stabilization difficult.
- Oblique fracture: The fracture line is angled across the bone shaft. While realignment is relatively straightforward, maintaining proper stabilization can be challenging.
- Comminuted fracture: The bone breaks into several fragments.
- Segmental fracture: The bone is broken into two or more distinct segments.
Figure 1: Types of fracture lines — A. Transverse B. Spiral C. Oblique D. Comminuted E. Segmental
Bone fractures may also be categorized based on location, mechanism of injury, or the degree of displacement of bone fragments.
III. Causes
Bones usually fracture due to two main causes: trauma or underlying medical conditions.
3.1. Traumatic Causes
A traumatic fracture occurs when a force is applied to the bone that exceeds its ability to withstand the stress. There are several situations that can lead to traumatic fractures, such as: falling from a certain height; severe impact in motor vehicle accidents or sports injuries; a heavy force compressing the bone, such as being struck by a falling object; or the bone being bent at an unnatural angle, for example, when the leg twists suddenly or is forcefully turned.
3.2. Pathological Causes
A pathological fracture is a condition in which the bone has reduced mineral density, making it weak, brittle, and more susceptible to breaking under external force (even if the force is mild or normal). Some medical conditions that may increase the risk of fractures include:
- Osteoporosis: A condition characterized by decreased bone mineral density. This is the most common cause of fractures in older adults.
- Bone tumors: Both benign and malignant tumors can weaken the bone structure, making it more prone to fractures.
- Hypercalcemia: Elevated calcium levels stimulate bones to release too much calcium, leading to osteoporosis and bone weakness.
- Myelodysplastic syndromes: A disorder in which the bone marrow does not produce enough healthy blood cells to nourish the bones, causing bone weakness from within.
IV. Treatment of Bone Fractures
4.1. Mechanism of Fracture Treatment
The treatment approach will depend on the severity and location of the fracture. In addition, age and medical history may also affect the recovery process.
During the healing process, new bone forms around the fractured fragments. If properly aligned and stabilized, the new bone will develop and fuse with the broken bone. Therefore, the fundamental principle in fracture treatment is to realign the bone to its correct position and keep it immobilized until complete healing occurs.
4.2. Common Methods of Fracture Treatment:
- Casting: Casts made from plaster or fiberglass form a rigid protective layer that covers the fractured area. Casting is commonly used in cases that require immobilization for several weeks.
- Splinting: A splint is used to immobilize one side of the fractured bone. This method is often applied for closed fractures.
- External fixation: In this procedure, the doctor inserts metal pins or screws above and below the fractured bone. These pins are connected to a metal frame outside the skin to keep the bone from shifting during the healing process.
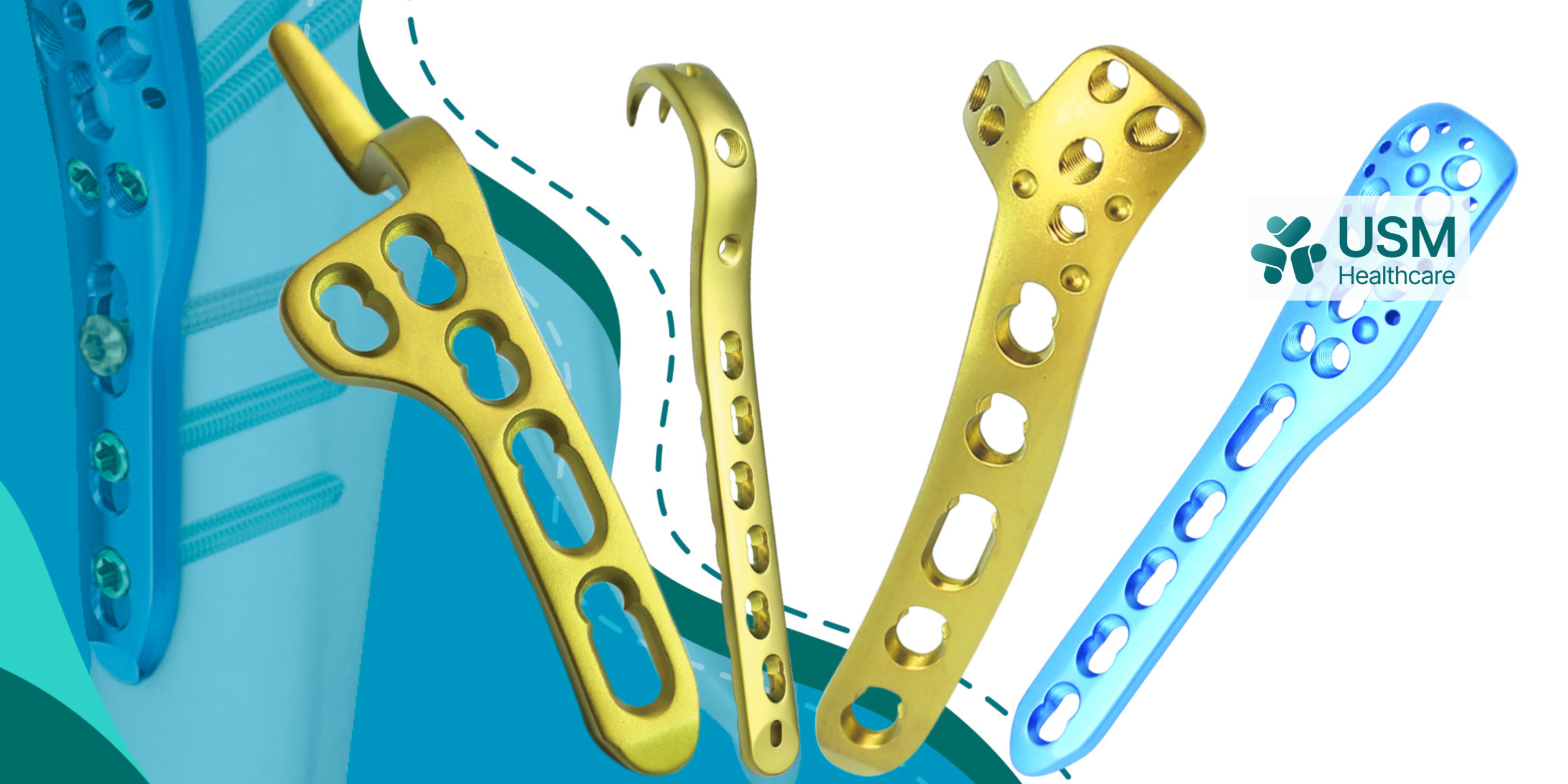
- Open reduction and internal fixation (ORIF): Typically used for complex fractures. In this case, through a surgical incision, the surgeon will realign the broken bone internally and then secure it with screws or metal plates placed directly on the bone surface.
Figure 2: Bone stabilized with screws or metal plates
- Joint replacement: This method is indicated when the fracture severely damages the upper part of the femur or the femoral neck in elderly patients.
- Bone grafting or bone fusion: This technique is used when the gap between bone fragments is too large. It may also be indicated in cases of delayed healing or nonunion fractures.
- For minor fractures, such as those in fingers or toes, treatment may involve external manipulation without the need for casting.
In addition, to promote recovery, patients may need to adjust their daily habits, ensure adequate rest, and limit movement of the injured area until the fracture site is fully healed. Prolonged immobilization of a body part can lead to muscle weakness and limited range of motion. Therefore, after the initial treatment phase, patients may be advised to undergo physical therapy to restore function to the fractured area.
Figure 3: Physical therapy exercises to accelerate bone healing
References:
https://www.gleneagles.com.sg/vi/conditions-diseases/fractures/symptoms-causes
https://tamanhhospital.vn/gay-xuong/https://www.msdmanuals.com/vi-vn/professional
https://th.hopluchospital.com/gay-xuong-ho-nguyen-nhan-trieu-chung-va-cach-dieu-tri/
https://hellobacsi.com/benh-co-xuong-khop/ran-xuong-gay-xuong/gay-xuong/